Experts say childhood exposure to domestic violence can impact health in adulthood
As October highlights Domestic Violence Awareness Month, psychologists and Helpmate of Asheville say adverse childhood experiences can have long term health impacts, which can be mitigated by building resiliency.
“Just seeing it is often as powerful as experiencing it,” said Pamela Laughon, associate professor of psychology at UNC Asheville.
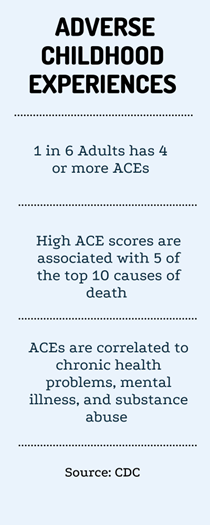
Officials at the CDC define certain traumatic events as those occurring until the age of 17, such as witnessing or experiencing violence in the home, as ACEs, or adverse childhood experiences.
“People who experience domestic violence, which is one of the categories of ACEs, as children are both more likely to be victims of intimate partner violence as adults and they are also more likely to experience more severe forms of PTSD,” Alice Beecher, youth outreach specialist for Helpmate of Asheville said.
The ACEs questionnaire was originally developed in the ‘90s as a 10-item scale, and it can predict the rate of physical illness a person has in their adulthood, Laughon said.
“ACEs are very, very common,” said Certified Prevention Specialist and former Licensed Clinical Addictions Specialist Patti Tiberi. “Even when you think about people who are well off in life, they might still have a high score.”
Officials at the CDC report over 61% of adults experienced at least one ACE, and 1 in 6 experienced over 4 ACEs.
Tiberi said everyone can benefit from knowing their ACE score. Although the ACE quiz is available on Google, Tiberi said a person who plans to take the ACE quiz should involve their support system in the process.
“It’s important you let somebody in your circle know that you’re going to try this,” Tiberi said. “These are very personal questions and some of us might get triggered as we complete the test.”
Officials at the CDC include exposure to domestic violence in the home on the ACE questionnaire along with other traumatic experiences such as abuse or neglect, a family member’s suicide, a family member’s incarceration, parental substance abuse and/or having a parent with mental illness.
“This is not, ‘Woe is me, I’ve had a lot of trauma,’ but it is hopefully beginning a discussion about ‘I’ve lived through a lot of difficult stuff, and I need to be able to find a way to manage it
differently to help my body heal so that I don’t end up getting sick with a lot of different chronic diseases,’“ Tiberi said.
Tiberi said chronic exposure to ACEs in childhood can trigger the amygdala to stay on constant alert. The amygdala is like the brain’s smoke detector, and it constantly scans the environment for safety. When it cannot find safety in its environment, it triggers the fight, flight, freeze reaction which floods the body with stress chemicals.
“Your breathing changes, your muscle tone changes — everything. There’s not one system in the body that’s not impacted by fight or flight,” Tiberi said.
When the amygdala is engaged in this reaction, the brain cannot perform executive functions such as decision-making and planning, Tiberi said. This can lead individuals with high ACE scores to experience out-of-control emotions and have problems paying attention.
Beecher said people sometimes respond to reading about ACEs by feeling depressed, but there is also a whole other assessment called the Positive Childhood Experience Scale. Studies show these experiences mitigate the effects of ACEs.
“The neuroplasticity of the brain is amazing,” Beecher said. “Just having one teacher that you really trusted, for example, can be something really transformational or set the template for being able to develop those healthier relationships as an adult.”
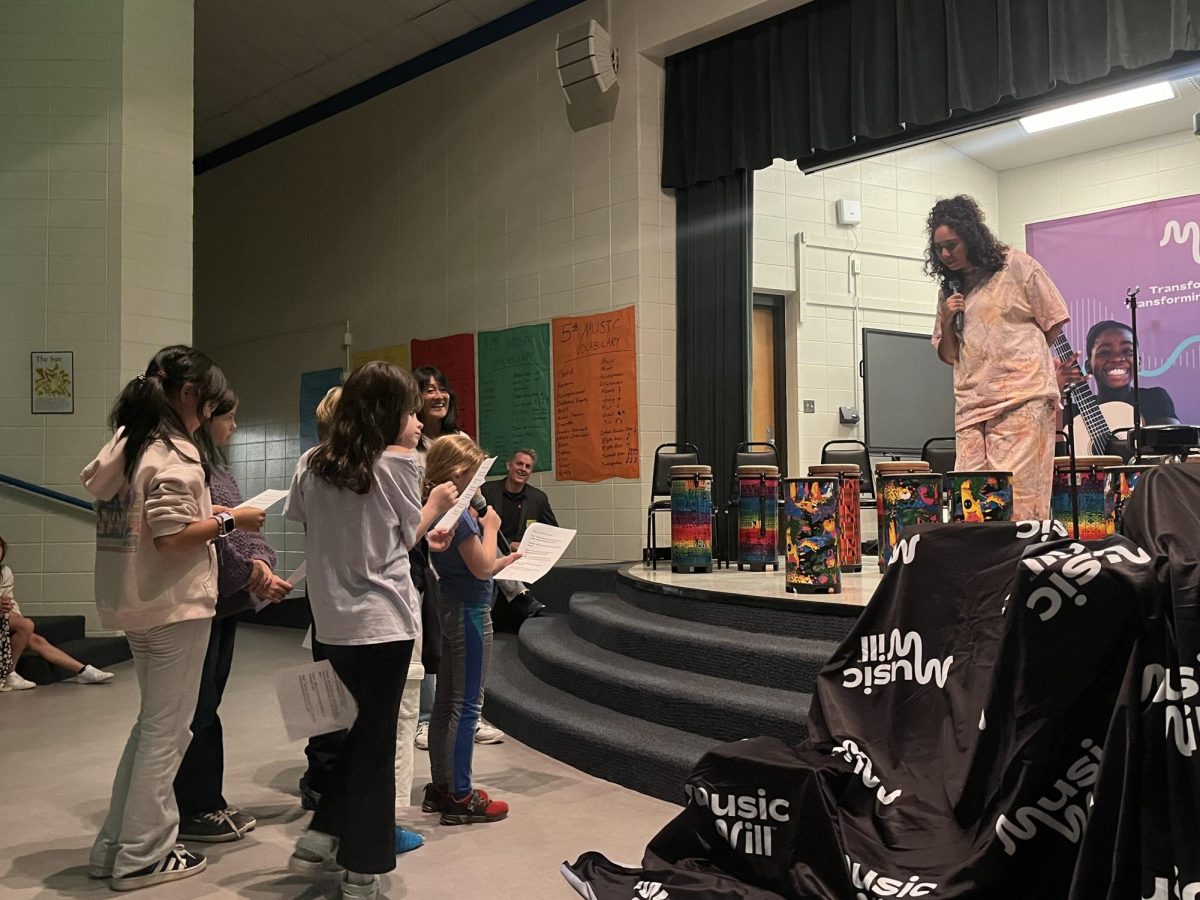
Laughon said researchers are studying resilience and have published hundreds of studies on the kinds of experiences children need to be resilient. She said people with high resiliency, or the ability to bounce back from stressors, do really well despite having high ACE scores. Tiberi said participating in creative arts or meditation are a couple of examples of activities that build resilience.
“Resilience skills help you step back, reset your nervous system,” Tiberi said. “But if you didn’t grow up seeing those modeled by somebody then you have to learn. A lot of times that’s where mentors come in, teachers, counselors.”
Tiberi said she supports people creating a recovery plan for themselves, especially when things are going relatively well. She said traditional talk therapy helps people who are more verbal while somatic therapy benefits those who are having more troubling body sensations.
“If I learned a skill that allows me to reconnect with my executive function, my nervous system automatically goes to a chill place. And now the adrenals calm down, the breathing regulates, the heartbeat slows down, the oxygen intake increases, all these kinds of things,” Tiberi said. “Which means that all of those chemicals that we don’t need in our bodies will be flushed.”
Laughon said cognitive behavioral therapy, or CBT, can help people with PTSD because it trains the mind to think differently.
Beecher said finding a way to work through difficult emotions like shame with a trauma-informed therapist or in a support group can help.
“I think that’s the main thing with trauma. Safe connections and safe relationships are so much of how people do heal,” Beecher said.
“It’s important to know that ACES are not fate. They’re not your destiny. You can change the impact of those anywhere along your journey,” Tiberi said.